Blood tests of several people who were in contact with a patient in Missouri who caught H5N1 bird flu without any known exposure to infected animals reveal at least one of them — a person who lived in the same house and had symptoms at the same time — also had the virus, according to two sources with knowledge of the investigation.
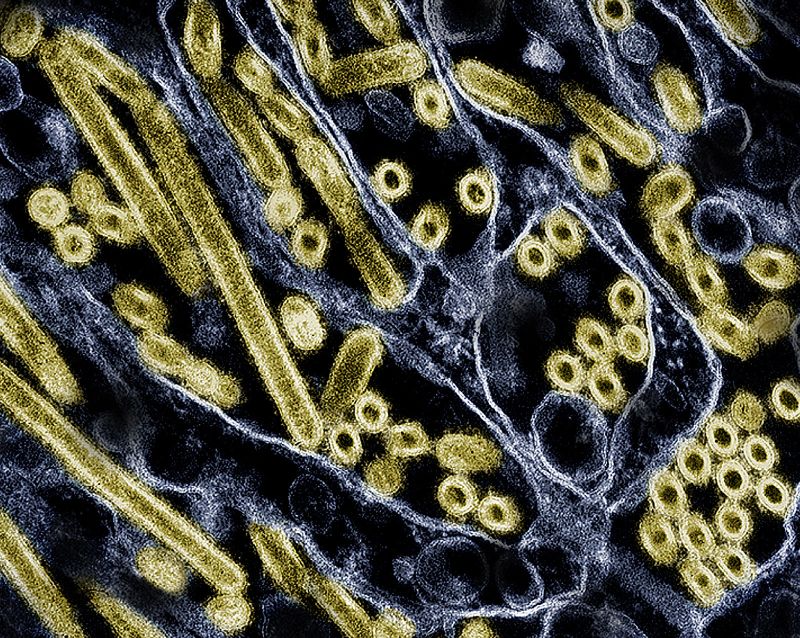
H5N1 is a type of influenza that’s rare in people, but is highly contagious and deadly in several species of animals, including poultry and dairy cattle, raising fears that it could mutate and become a virus that preys on people, too.
The specialized blood tests, which were conducted by scientists at the US Centers for Disease Control and Prevention in Atlanta, looked for immune proteins called antibodies made in response to an infection. These antibodies confirm that a person has had a past infection with a particular pathogen. The results are expected to be shared more widely with public health officials, scientists and the media in several calls hosted by health officials on Thursday morning.
The tests were conducted to understand whether the Missouri patient – who is the first person to catch H5N1 influenza in the United States without any apparent exposure to infected animals – infected anyone else. So far, the H5N1 virus has not been able to spread easily between people. Infectious disease experts fear that if the virus gains that ability, it could touch off a new pandemic.
While the results don’t rule out human-to-human transmission of the virus, they do suggest it isn’t widespread and that it didn’t happen in a health-care setting where caregivers have close physical contact with patients.
Around the United States, more than two dozen people have tested positive for H5N1 flu so far this year and nearly all of them have reported exposure to infected dairy cows or chickens, according to the CDC.
Source of the infections is still a mystery
The new test results show that the health-care workers who developed symptoms of respiratory illness after caring for the patient — before doctors were aware of the H5N1 infection — were negative for antibodies against the infection. However, a person who lived in the same house with the patient and got sick and the same time did have antibodies to H5N1 infection.
Infectious disease experts with knowledge of the findings said it was a relief to see the results.
“I am very reassured by the fact that the health-care workers were not positive, and that gives me a lot more confidence that this is not really spreading in a sustained way between people,” said Dr. Jennifer Nuzzo, who directs the Pandemic Center at the Brown University School of Public Health.
At the same time, Nuzzo said, information gaps limit what can be learned about how both the patient and a member of their household became ill.
Experts say that because both people began having symptoms at roughly the same time, it’s more likely that they shared a common exposure instead of one person giving it to the other, but person-to-person transmission in that case can’t be ruled out.
“We’re still left with all those questions,” said Dr. Michael Osterholm, who directs the Center for Infectious Disease Research and Policy at the University of Minnesota. “Was it the same source? Was it person to person?”
Another question relates to symptoms. Both people who tested positive for H5N1 didn’t have typical flu symptoms. Instead, they had gastrointestinal issues, including diarrhea, which initially led investigators to suspect food poisoning might be the cause of their simultaneous illnesses.
Osterholm said it’s unclear whether the H5N1 virus was causing those symptoms or whether they might have had more than one infection at the same time.
“I’ve seen that happen before,” he said.
Both the Missouri patient and their household member have been interviewed several times about potential exposures to the virus. Neither has indicated they had any raw milk or other raw dairy products, and neither could recall any contact with potentially infected animals, including “direct or indirect contact with wild birds, domestic poultry, cats, cattle including no consumption of raw dairy products, or other wildlife by the case and close contacts,” said Lisa Cox, a spokesperson for the Missouri Department of Health and Senior Services, in an email. The Missouri Department of Health and Senior Services has been leading the investigation with assistance from the CDC.
Experts said the test results shed little light on how both people caught the virus.
“I don’t think we’re going to get good data out of it to tell us much,” said Dr. Rick Bright, an immunologist and vaccine researcher who previously led the Biomedical Advanced Research and Development Authority.
Bright said it would be an important case to keep bookmarked in the event that similar instances come to light that might suggest the virus is causing unusual symptoms or perhaps is infecting people through a route of exposure that hasn’t yet been recognized.
“There are so many weird things about this one, I don’t think we can put a lot of weight in it,” Bright said, though he added that the CDC did a thorough job looking for antibodies in the case. He said the fact that the health-care workers did not test positive was both “convincing and comforting.”
Searching for evidence of past infections
In order to get these test results, the CDC had to reconstruct the exact virus carried by the patient in Missouri in order to look for antibodies that might attach to its unique structure. The agency explained in a recent news briefing that it was taking those extra steps to avoid falsely negative or falsely positive results.
- Sign up here to get The Results Are In with Dr. Sanjay Gupta every Friday from the CNN Health team.
The extra efforts increased the agency’s confidence in its findings, but it also added another delay to a case that took weeks to be identified and investigated. The patient was originally hospitalized on August 22.
The delays, while perhaps unavoidable, have frustrated preparedness experts who say any system that takes this long to identify and track infections hamper the country’s ability to respond should H5N1 infections become more widespread.
“I am thrilled that we’re finally getting data that should have been shared weeks ago. I think every case, every human case of H5 is an important case. They’re all valid and they’re all worth [blood testing], because this is a virus that should not be in a human host and is one that we need to better understand so that we can prevent possible human-to-human transmission,” said Dr. Erin Sorrell, who is a senior scholar at the Johns Hopkins Center for Health Security.
“Every data point is essential at this point in the process,” Sorrell said. “So just that delay, I think, is a massive, massive issue.”